Blend traditional and digital impressioning for an easier transition
Samer S. Alassaad, DDS | James W. Childress, DDS | Stacie Rodriguez, RDAEF2
CAD/CAM restorative technology is neither a fictitious nor a futuristic idea anymore because in-office CAD/CAM is already a reality.1 Its popularity is increasing in private practices as well as in dental laboratories; recent research and case reports demonstrate the high-quality restorations it can produce in terms of marginal adaptation, longevity, function, and esthetics, thereby ushering in a new era in the delivery of dentistry.2-6
A commonly expressed concern about this technology is the learning curve involved in immediately producing high-quality results regardless of the system used.6-8 Although it remains unclear what impact a steep learning curve has on overall results, research presented at the 2012 American Association for Dental Research Annual Meeting demonstrated how minimal operator training and experience can have an adverse effect on digital impressions in terms of the marginal gap of restorations.9
Once a CAD/CAM system is acquired, it is emphasized that the clinical team immediately scan prepared teeth intraorally and then design, mill, stain, and glaze restorations in a single visit while the patient is in the dental chair. After the initial training, the clinician with minimal experience faces the question of whether the clinical team is then ready to make chairside restorations with optimal fit, function, and esthetics.
On the other hand, dentists have used traditional impressions and models to fabricate well-fitting and long-lasting restorations for decades.10,11 This approach is familiar, and models and dies provide the ability to evaluate marginal fit, contour, and interproximal and occlusal contacts prior to cementing restorations.
In the initial stages of integrating CAD/CAM, therefore, using accurate conventional impressions and stone models to scan prepared teeth can facilitate a smoother transition to chairside scanning and milling as the dentist and the clinical team become more familiar and comfortable with all phases of this technology. The time needed and the number of patients to be treated using this approach will vary from one practice to another, depending on the goals and the comfort level of the clinical team. Although this approach may be viewed as “backward thinking,” it helps overcome the challenges faced by the novice user while maintaining better control over the end results, especially when immediate implementation of this technology is crucial.
The advent of CAD/CAM technology promised many potential benefits, including same-day, durable, and well-fitting restorations and full control and delivery of restorative services without laboratory involvement. These promises have proved possible; however, CAD/CAM technology is not a one-click magical system yet. Many challenges are still faced by the novice user at different stages of this technology’s initial integration.
As with other indirect restorations, teeth restored with CAD/CAM require good preparation.12 Meticulous attention to preparation criteria is paramount. Traditionally, lab technicians were able to manage imperfections in tooth preparations and still produce well-fitting restorations. Imperfections such as sharp transitions and edges at the preparation margin can adversely influence the final fit of milled restorations. Clinicians need to practice more ideal tooth preparation regardless of the method of scanning, either intraorally or from a model. Once intraoral scanning is used, clinicians will also have the opportunity to immediately evaluate their preparation design and correct any visible imperfections.
Digital impressions have many advantages over conventional impressions.8 They eliminate impression distortion and bubbles, errors in pouring models, and chipping margins of dies during fabrication. They also reduce gagging reflex of patients. However, digital impressions still require adequate soft tissue retraction and a well-isolated field free of blood and saliva. They have their own challenges in terms of capturing preparation margins in certain situations, including deep subgingival margins and margins with minimal interproximal clearance. Although the improved durability and inherent esthetics of porcelain restorations gave clinicians the ability to make esthetic supragingival restorations and thus make impression-making easier both digitally and conventionally, producing accurate impressions still requires adherence to strict protocols.
Although we currently live in a digital age, the process of becoming familiar with CAD/CAM software can still be overwhelming; it requires practice and time to perform the necessary tasks seamlessly.13 Most of the initial training is performed on stone models that have ideal occlusion, ideal alignment, and a preoperative model of ideal tooth contours, which is not the norm in daily clinical practice. Designing full-crown restorations for less than ideal tooth conditions (eg, rotated teeth, teeth with long axial walls, severely damaged teeth, teeth that have old restorations with inadequate contours) will be more time consuming initially, as the digital system may not necessarily provide the ideal design automatically.
The final stage of fabricating CAD/CAM restorations is staining and glazing. For the beginner, this stage can be very challenging.14 Dentists traditionally have referred the fabrication of porcelain restorations, including staining and glazing, to lab technicians. In everyday practice, dentists mostly use composite resin to create immediate esthetic restorations; these differ from porcelain restorations.
Posterior CAD/CAM porcelain blocks are monochromatic; they come only in one shade per block. Matching posterior restorations to adjacent teeth in terms of the gradation of chroma and value is achieved mostly through surface staining. Currently, multi-shade CAD/CAM porcelain blocks are only available for IPS Empress® porcelain material (Ivoclar Vivadent, www.ivoclarvivadent.com), which is only suited for anterior restorations due to its limited strength.
The key to the final esthetic outcome is mixing stains in the right consistency and applying the staining and glazing strokes to create an even layer without incorporating bubbles and without the stains bleeding into each other. Additionally, staining and glazing porcelain (IPS e.max® CAD, Ivoclar Vivadent) currently requires firing in a porcelain oven (Programat® CS, Ivoclar Vivadent) for approximately 20 minutes, excluding the cooling time needed before trying the restoration in the patient’s mouth.
In the initial phases of integrating this technology, it is less stressful to the minimally experienced clinical team to work on models without having the patient waiting in the dental chair. Clinicians can then evaluate each finished restoration thoroughly and closely in terms of marginal fit, contour, and interproximal and occlusal contacts. They can also investigate the possible causes of any undesired outcome and have a better chance to make any adjustments. Staining restorations can be performed using clinical photographs of the selected shade and adjacent teeth. As the team becomes more familiar with all the phases of the CAD/CAM system, selecting ideal cases for chairside scanning and milling, such as restorations with supragingival margins and those that are outside the esthetic zone and with ideal preoperative contours, will test the readiness of the team for complete chairside digital dentistry and ensure more predictable results.
In the meantime, continuously seeking additional educational opportunities will also help speed up this learning curve. This includes, but is not limited to, courses provided by manufacturers or independent institutions, online resources such as educational videos, additional in-office training by CAD/CAM training specialists, and participating in study clubs and CAD/CAM communities.
Diagnosis and Treatment Planning
A 57-year-old healthy patient presented with asymptomatic mesial marginal ridge and mesio-buccal cracks accepting methylene blue dye in addition to a deteriorating disto-occlusal amalgam restoration in tooth No. 4 (Figure 1 and Figure 2). Upon removal of the old restoration, methylene blue dye was used again to highlight the extension of the cracks. A pulpal floor crack and a buccal cusp crack were noted, thus requiring a full-coverage restoration (Figure 3).
Tooth Preparation
Irregularities in the tooth structure were filled with a core build-up composite (LuxaCore®, DMG America, www.dmg-america.com) bonded with a single-component bonding agent (Adper™ Single Bond Plus, 3M ESPE, www.3mespe.com) after etching with 38% phosphoric acid etching gel (Etch-Rite™, Pulpdent, www.pulpdent.com). Axial and occlusal tooth reduction for full porcelain crown restoration was achieved by a round-end cylinder bur (NeoDiamond® KS1, Microcopy, www.microsopydental.com). The modified shoulder margin with rounded internal angle was finished by a medium-grit diamond cylindrical-end cutting bur (10839.31.014, Brasseler USA, www.brasselerusa.com) to remove any troughed edges on the margin; this final step of the tooth preparation is performed at minimum speed with air cooling for better visualization of an ideal margin (Figure 4).
Conventional Impression and Model Making
After crown preparation, soft tissue retraction was obtained by knitted retraction cords (Ultrapak® E™, Ultradent Products, Inc., www.ultradent.com) soaked in buffered aluminum chloride hemostatic solution (Hemodent®, Premier Dental, www.premusa.com). A con-
ventional vinyl polysiloxane (VPS) impression was made using light-body VPS (Reprosil®, DENTSPLY Caulk, www.caulk.com) and heavy-body VPS (Genie® VPS, Sultan Healthcare) impression materials in a metal triple tray (Quad-Tray® Xtreme™, Clinician’s Choice, www.clinicianschoice.com) (Figure 5). A bite record limited to the prepared tooth was made with VPS bite registration material (Blu-Bite®, Henry Schein, www.henryschein.com). The patient was dismissed with a temporary crown restoration (Luxatemp® Automix Plus, DMG America) cemented with temporary cement (TempBond®, Kerr Dental, www.kerrdental.com).
The impression was disinfected with intermediate-level surface disinfectant (CaviCide®, Metrex, www.metrex.com) and then rinsed under cold tap water and air dried thoroughly. Additional light-body VPS was carefully injected around the subgingival areas of the impression to create a trimmed die for better scanning results (Figure 6).
Although this additional step does not simulate oral conditions, it will facilitate digital scanning in the initial phase of integrating this technology. The impression was allowed to bench set for 3 hours. Surfactant (DeLar Surfactant, DeLar Corporation, www.delar.com) was lightly sprayed to reduce voids in the poured stone. Two models were poured with die stone (Die-Keen® Green, Heraeus Kulzer, www.heraus-dental-us.com) and mixed with hardener (Gypsum Hardener, Whip Mix, www.whipmix.com) in a vacuum mixer (Twister pro, Renfert USA,www.renfert.com) (Figure 7). One solid model was used for digital scanning and later for mounting models and checking interproximal and occlusal contacts of the milled restoration. The other model was used for a separate die preparation for the evaluation of the margins and contours of the milled restoration.
Upper and lower models were mounted on a plastic glue-on single-use articulator (“ArtiQuick,” Dental Ventures of America, Inc., www.dentalventures.com). The die was trimmed around the margin with carbide lab bur (Robot® Carbide HP Cutter SH 77E, Shofu Dental Corporation, www.shofu.com), and then coated with a die hardener (Clear Coat®, American Dental Supply, www.americandentalsupply.net) to reduce fracture of the die margin. The margin was later marked with a red pencil.
Digital Restorative Technique
The prepared tooth and at least two adjacent teeth were digitally scanned into a CAD/CAM dental system (E4D Dentist™ System, D4D Technologies, www.e4d.com) (Figure 8). The bite record taken in the patient’s mouth was placed over the solid model and was also digitally scanned. Once the digital scans were obtained and stored via the software, the restoration margins were demarcated (Figure 9) and the restoration was designed to the desired contour and occlusal and interproximal contacts (Figure 10 and Figure 11).
Careful attention needs to be paid to the ripples at the margin areas; understanding how to work with this different medium in terms of the way digital restorations look is crucial to their success. Keeping the ripples that are naturally added by the software or even adding them if they are not adequate will prevent marginal porcelain chipping during the milling process.
The restoration was milled out of a lithium-disilicate glass-ceramic block (IPS e.max® CAD). While the restoration was still in the precrystallized state, it was evaluated for interproximal and occlusal contact, contour, and marginal adaptation. Interproximal contacts were evaluated by marking the interproximal sufaces of the solid model with a lead pencil. These markings will transfer to the premature areas of interproximal contacts of the crown restoration and then will be adjusted as needed until the restoration is completely seated (Figure 12). Occlusal contacts were evaulated by an articulation paper and adjusted as needed. Occlusal grooves were further defined with a lab Tri-Fissure carbide bur (Premier Dental). The crown restoration margins were evaluated on the trimmed die for marginal gaps, short margins, and excess margins along with the overall crown restoration countours (Figure 13).
Adjustments were made as needed with a lab diamond bur (Two Striper® TSZTECH™ X590.12Z, Premier Dental) and a flame-shaped diamond green stone lab bur (Dura-Green®, Shofu Dental). The crown restoration was crystalized, then stained and glazed to the desired esthetics.
Final Cementation at a Second Appointment
The restoration was evaluated in the patient mouth for marginal fit, interproximal contacts, occlusal contacts, and esthetics. Needed adjustments were made, which at this stage were very minimal. The restoration was etched for 20 seconds with an IPS ceramic etching gel and primed with a ceramic primer (Monobond Plus, Ivoclar Vivadent). Prior to cementation, the tooth surface was treated with a desensitizing agent (MicroPrime, Danville, www.danvillematerials.com). Finally, the restoration was cemented with self-adhesive resin cement (RelyX™ Unicem 2 Automix, 3M ESPE) (Figure 14 and Figure 15).
A postoperative radiograph was taken verifying excellent marginal fit and contour (Figure 16). All clinical procedures and laboratory evaluation and adjustments of the resoration were performed under 4.8x magnifcation (HiRes® Plus 4H, Orascoptic, www.orascoptic.com) and LED headlight (Zeon Discovery™, Orascoptic).
Using accurate stone models and dies in the initial phase of integrating CAD/CAM restorative technology provides peace of mind and better control over the end product. The practitioner and the clinical team can move towards complete intraoral scanning and chairside milling once they feel that they have acquired the skills necessary to deliver long-lasting ceramic restorations in a single visit.
1. Christensen GJ . In-office CAD/CAM milling of restorations: the future? J Am Dent Assoc. 2008;139(1):83-85.
2. Reich S, Gozdowski S, Trentzsch L, et al. Marginal fit of heat-pressed vs. CAD/CAM processed all-ceramic onlays using a milling unit prototype . Oper Dent. 2008;33(6):644-650.
3. Wittneben JG, Wright RF, Weber HP, Gallucci GO. A systematic review of the clinical performance of CAD/CAM single-tooth restorations . Int J Prosthodont. 2009;22(5):466-471.
4. Fasbinder DJ. Clinical performance of chairside CAD/CAM restorations . J Am Dent Assoc. 2006;(137 suppl):S22-S31.
5. Herrguth M, Wichmann M, Reich S. The aesthetics of all-ceramic veneered and monolithic CAD/CAM crowns . J Oral Rehabil. 2005;32(10):747-752.
6. Harsono M, Simon J, Stein J, Kugel G. Evolution of Chairside CAD/CAM Dentistry . Inside Dentistry. 2012;8(10):76-81.
7. Trost L, Stines S, Burt L. Making informed decisions about incorporating a CAD/CAM system into dental practice . J Am Dent Assoc. 2006;(137 suppl):S32-S36.
8. Stover J. Successfully integrating digital impressions into the practice . Inside Dental Assisting. 2012;8(2). www.dentalaegis.com/ida/2012/04/integrating-digital-impressions-into-a-practice. Accessed on January 24, 2013.
9. Kugel G, Beyari M, Lamfon H, et al. Marginal/internal crown fit evaluation of CAD/CAM versus press-laboratory all-ceramic crown [abstract 1366]. Presented at: AADR Annual Meeting; March 24, 2012; Tampa, Florida.
10. Hamalian TA, Nasr E, Chidiac JJ. Impression materials in fixed prosthodontics: influence of choice on clinical procedure . J Prosthodont. 2011;20(2):153-160.
11. Raigrodski AJ, Dogan S, Mancl LA, Heindl H. A clinical comparison of two vinyl polysiloxane impression materials using the one-step technique . J Prosthet Dent. 2009;102(3):179-186.
12. McLaren E. CAD/CAM dental technology: a perspective on its evolution and status . Compend Contin Educ Dent. 2011;32(4):74-75.
13. Christensen GJ . Is now the time to purchase an in-office CAD/CAM device? J Am Dent Assoc. 2006;137(2):235-236, 238.
14. Helvey GA. Chairside CAD/CAM . Inside Dentistry. 2009;5(10):58-67.


Figure 1 Figure 2 Figure 3


Figure 4 Figure 5 Figure 6


Figure 7 Figure 8 Figure 9
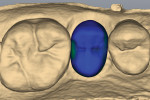
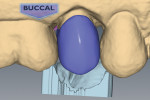
Figure 10 Figure 11 Figure 12
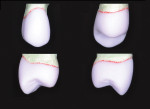

Figure 13 Figure 14 Figure 15
Figure 16