Case report describes a procedure in which the molars were in close
relationship with the inferior alveolar nerve.
By Giuseppe Monaco, DMD | Giselle de Santis, DMD | Michele Diazzi, DMD | Claudio Marchetti, MD, DDS
In this case report, the authors discuss the technique of coronectomy in a 50-year-old patient with previous episodes of pericoronitis. As shown on the cone beam computed tomography (CBCT), the third molar root was in close proximity to the inferior alveolar nerve (IAN). Here, the authors highlight some surgical steps of the protocol that are crucial to the final clinical result. Following this surgical protocol, the authors have performed 85 coronectomies without any instances of intra-operatory failure after nearly 2 years of follow-up.1
Coronectomy was first proposed in 19842 as surgical alternative to a complete extraction in cases involving mandibular impacted third molars in close proximity to the IAN. In a study published in April 2012,1 the authors reported on 43 coronectomies of inferior third molars that present a 2 year follow-up. Among these patients, two patients underwent a second surgery to remove the previously sectioned roots—after 10 months and 1 year, respectively. Prior to the second surgery, the first patient complained of intermittent pain; the other patient was completely asymptomatic. In neither case were there neurological injuries to the patient as a result of removal of the root fragments, because the root fragment had migrated from the mandibular canal. During the follow-up period, none of the patients reported fever. Alveolitis was reported in only one coronectomy; it occurred 15 days after the surgery. This case was treated with antibiotic therapy, after which the patient did not report any further complications.
The authors strongly believe that the ability and the surgical experience of the operator is crucial to the final outcome.
Diagnosis
Coronectomy should be planned after a CBCT radiograph confirms the actual proximity between the third molar roots and the alveolar nerve. Real proximity is defined as the absence of the cortical wall of the mandibular canal and the existence of an effective contact between the root and nerve. Note: Coronectomy cannot be performed if the third molar presents with deep caries.
Pharmacologic Therapy
The patient received antibiotic prophylaxis (2 g of amoxicillin in tablet form) 1 hour before surgery and postoperatively for 4 days (1 g every 8 hours). Starting the day after surgery, the patient rinsed twice a day with 0.2% chlorhexidine for 10 days. For postoperative pain, the patient was prescribed an anti-inflammatory agent: 600 mg of ibuprofen, two tablets daily.
Flap Design
When the tooth is partially impacted, in order to obtain a primary closure of the wound it is advisable to perform a triangular flap with a mesial releasing incision distal to the second molar. In this circumstance, the releasing incision is not repositioned, and the flap is sutured to the lingual side to obtain the closure.
In the case of a completely impacted tooth, it is easier to obtain a primary wound closure because there is sufficient gingival tissue, and the surgeon can choose either a triangular or envelope flap.
Osseous Surgery
After flap reflection, the ostectomy should be minimal to avoid the risk of root mobilization during crown resection. When the third molar is in the vertical position, it is possible to perform the crown resection without any osseous surgery.
Crown Resection
When the third molar is in a vertical position, the surgeon can use a fissure bur at an approximately 45° angle to obtain a superficial lingual cut 2 mm to 3 mm below the bony margin. With this mesio–distal dissection the surgeon avoids totally transecting the crown to the lingual plate in order to prevent injury to the lingual nerve. A second dissection in the bucco–lingual direction is advisable to obtain two small fragments, which can be gently removed with a tissue forceps.
If the third molar is in a horizontal position, it is necessary to perform more osseous surgery to visualize the crown that is sectioned in a bucco–lingual direction and in a mesio–distal direction. In this case, the crown section is similar to the protocol adopted for complete extraction. In cases of root mobilization, during crown dissection, the root should be extracted because the mobility can easily lead to infection of the alveolus.
After the crown removal, the third molar root is reduced using a round bur in a high-speed surgical drill so that the remaining root fragments are at least 3 mm to 4 mm below the crest of the lingual and buccal plates.
The exposed dental pulp is irrigated with saline solution and no endodontic treatment is necessary. Before suturing, a periapical radiograph should be taken.
Postoperative Follow-Up
In the study published,1 the authors reported that patients who had undergone coronectomy did not experience more pain in the postoperative week than ones treated with complete extractions.
The first follow-up radiograph should be taken 3 months after surgery. The clinical protocol tested at the Oral Surgery Department of the University of Bologna provides a periapical radiograph at 3, 6, and 12 months and twice annually for the following 4 years.
In young patients (≤ 26 years), the risk of root migration is higher and more common in the first 3 months. At 6 and 12 months, root migration decreases because bone apposition coronal to the root fragments inhibits root movement. If the root migration occurs, it usually indicates bone regeneration at the distal surface of the second molar, as in orthodontic-assisted extrusion.
Root migration may also cause the eruption of the root fragments in the oral cavity. In these cases, the extraction is uncomplicated because there is no proximity to the inferior alveolar nerve and the roots are mobile.
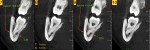
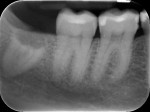
In this case, the preoperative radiographic evaluation involving CBCT imaging showed a close proximity between the inferior alveolar nerve and the third molar root (Figure 1 and Figure 2). According to the 2010 report by Susarla et al,3 when the cortical defect size of the mandibular canal is more than 3 mm, this extension of contact between root and IAN is associated with an increased risk of intraoperative nerve exposure. As is apparent in the preoperative photograph, the right mandibular third molar is partially impacted. In this clinical situation, it is better to perform a triangular flap with a mesial releasing incision distal to the second molar. With this type of flap, it is easier to obtain a primary closure of the surgical wound.
As shown in Figure 3, a vestibular triangular flap is raised with a minimal lingual flap. The authors do not perform ostectomy and the first cut of the crown is directed toward mesio–distal angulation. The fissure bur seen in this figure is used at an approximately 45º angle to obtain a lingual cut surface (from 2 mm to 3 mm) below the bony margin.
In this protocol, the surgeon does not totally transect the crown to the lingual plate in order to avoid injury to the lingual nerve.
The second dissection is carried out in a bucco–lingual direction in order to obtain two small fragments, which are gently removed using tissue forceps. With these two dissections—mesio–distal and bucco–lingual—the surgeon minimizes the risk of mobilizing the roots during the crown removal.
With the bucco–lingual dissection, the surgeon can also visualize the depth of the mesio–distal section and make the first cut deeper in a lingual direction, if necessary.
The distal fragment is then removed (Figure 4), and the tooth is reduced on the buccal surface at least 2 mm to 3 mm below the bony crest by a round bur in a high-speed surgical drill (Figure 5). With the mesio–distal section angled at 45º, it is usually not necessary to reduce the lingual surface.
Figure 6 shows the postoperative radiograph of the completed crown removal. In Figure 7, it is possible to see the primary closure of the wound obtained with a retraction of the vestibular flap to the lingual side without the repositioning of the mesial releasing incision. The procedure does not specify a reduction of the amount of attached gingiva around the second molar.
Photographs show tissue healing after 6 months (Figure 8); at 12 months, a small amount of root migration and bone apposition coronal to the root can be seen (Figure 9).
Coronectomy is an alternative surgical procedure that is safer than complete extraction when the third molar is in close proximity to the mandibular canal. The close proximity should be diagnosed by a CBCT or axial computed tomography.
After a coronectomy, root migration is generally an asymptomatic event, although in a few cases, it can indicate the eruption of the root fragments in the oral cavity. If the patient undergoes a second operation, the risk of experiencing neurological injuries is reduced.
The patient’s periodontal healing is generally improved, because the ostectomy necessary for crown resection is reduced compared to that necessary for complete extraction. Moreover, root migration, when present, induces bone apposition distal to the second molar in a manner that is similar to the one after orthodontic-assisted extraction.
1. Monaco G, De Santis G, Gatto MRA, et al. Coronectomy: a possible surgical option for impacted third molars in close proximity to the inferior alveolar nerve. J Am Dent Assoc. 2012;143(4):363-369.
2. Ecuyer J, Debien J. Deductions operatoires. Actualités Odonto-Stomatologiques. 1984;38(148):695-701.
3. Susarla SM, Sidhu HK, Avery LL, Dodson TB. Does computed tomographic assessment of inferior alveolar canal cortical integrity predict nerve exposure during third molar surgery? J Oral Maxillofac Surg. 2010;68(6):1296-1303.
Giuseppe Monaco, DMD
Visiting Professor
Department of Oral and Dental Science
University of Bologna
Bologna, Italy
Giselle de Santis, DMD
Clinical Fellow
Master in Oral and Implant Surgery
Department of Oral and Dental Science
University of Bologna
Bologna, Italy
Michele Diazzi, DMD
Clinical Fellow
Master in Oral and Implant Surgery
Department of Oral and Dental Science
University of Bologna
Bologna, Italy
Claudio Marchetti, MD, DDS
Professor of Maxillofacial Surgery
Department of Oral and Dental Science
University of Bologna
Bologna, Italy