Communication and correct diagnostic information are the keys to a successful outcome.
In the process of fabricating successful restorations, clear and detailed communication between the dentist and laboratory cannot be overemphasized. All of the diagnostic tools required should becomplete and specific upon delivery to the laboratory. When fabricating a full-mouth restoration, considerable information is required, including a periodontal chart; preoperative and provisional photographs and radiographs; master impressions; provisional impressions; a centric relation (CR) bite registration; a horizontal plane reference; and cementoenamel junction (CEJ) measurements. This case presented in this article demonstrates the level of collaboration that is essential between dentists and laboratory technicians to achieve a successful full-mouth restoration.
Tooth wear is an ordinary and commonplace occurrence, especially with aging. Wear impacts the patient’s foremost concern—esthetics. Loss of tooth structure can affect the shape, surface, and color of the teeth as well as the occlusion of the dentition, causing dentin hypersensitivity, pain and discouragement.
When tooth wear is a result of attrition, the occlusal surfaces are worn down from tooth-to-tooth contact from natural forces such as chewing, or pathological friction caused by bruxism.1,2 While emotional stress can be a precursor to bruxism, it is a mistake to consider it the only cause. Research indicates that occlusal interferences, however minor, can trigger bruxism, grinding, clenching, or gnashing of the teeth.2 Not only can malocclusion cause bruxism, teeth grinding can result in malocclusion. Grinding contracts the elevator muscles, overloading the teeth, supporting structures, and the temporomanibular joints (TMJ), causing pain and wear.
To help ensure lasting restorations, occlusal balance must be restored. Occlusal harmony eliminates incoordination of the jaw musculature. When the jaw muscles are in harmony and there is no premature contact of the teeth, occlusal stability has been achieved. Therefore, posterior interferences to centric relation should be eliminated and anterior guidance established.2
Today, while focusing on preserving sound tooth structure, many laboratory ceramists and dentists use the additive model as a conservative, less-invasive technique for providing lasting results.3 The importance of choosing an appropriate restorative material for additive treatment cannot be overemphasized; the restorative material should promote conservative dentistry, provide superior wear resistance, be durable and long-lasting to avoid the need for re-restoration, and provide an esthetically pleasing smile. Various advanced materials are available that allow ceramists and dentists to provide long-lasting, esthetic restorations while practicing conservative dentistry.
A 50-year-old, highly stressed businessman presented with severe wear on all of his teeth, which developed over the years due to a combination of age and malocclusion (Figure 1). After the initial examination and consultation, the patient agreed to treatment in three phases using lithium-disilicate all-ceramic restorations (IPS e.max® Press, Ivoclar Vivadent, www.ivoclarvivadent.com).
Treatment Plan
Veneers were planned for the anteriors. PFM crowns had been previously placed on the patient’s posteriors, as well as some very large restorations. Therefore, crowns were indicated for the posteriors. The treatment plan involved correcting the occlusion, opening the bite, and providing cosmetic restorations.
IPS e.max provides the fit and function of traditional pressable ceramics, and its unique lithium-disilicate structure—including its controlled size, shape, and density—ensures greater strength and durability.4-7 IPS e.max Press also provides superior performance for pressing all-ceramic restorations intended for cut-back and layering techniques.8
With a flexural strength of 400 MPa and manufactured with approximately 70% by-volume needle-like crystals in a glassy matrix, lithium disilicate ensures predictable and long-lasting restorations, is suitable for the most complex cases, and demonstrates lifelike translucency for esthetically challenging cases.9-13
Diagnostics
Because of the patient’s unusual request to.complete the rehabilitation in three phases and the necessity to open the bite, the occlusal stability of the provisionals would be impossible to gauge because they would never be in place at the same time. Therefore, an evaluation of the joint vibrations was done to assess the health and function of the TMJs.
A full periodontal charting and a full set of diagnostic photographs and radiographs were taken. A polyvinyl siloxane (PVS) impression material (Imprint™, 3M ESPE, www.3mespe.com) was used for the upper and lower impressions. The characteristics of PVS allow for multiple pours of diagnostic models. The impressions also facilitate creation of a model of the initial and final restorations on the articulator (Stratos®, Ivoclar Vivadent).
A CR bite registration was taken after the patient had worn an anterior deprogrammer for 5 days. New vertical dimensions were determined and a reproducible condylar position was captured.14 Proper vertical dimensions were further established using upper and lower incisor CEJ-to-CEJ measurements from digital calipers. This information enabled the ceramist to mount the casts in centric relation and correct the patient’s vertical dimension. With the addition of clinical photographs, the ceramist produced a precision wax-up.
Additive/Reductive Model
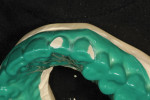
Following the additive/reductive diagnostic model technique developed by Culp, after the diagnostic models were poured and based they were mounted using CR bites and an earless facebow (Figure 2) (Kois Dento-Facial Analyzer, Panadent, www.panadent.com) with the Stratos/Kois mounting table on a Stratos 200 articulator. A green plastic suck-down material (LAK Enterprises, www.lakdental.com) was vacuum-formed over the preoperative model. Any dentition protruding from arch form (labially or lingually) was reduced, creating a reduction stint used intraorally to enable the dentition to conform to the proper arch form. The preparations were completed and the final margin positions were established and smoothed with the KS3SC, KS5SC, KS6SC, and 8856.021 burs (KOMET USA, www.kometusa.com).
After highlighting these reductions on the preoperative model (Figure 3 and Figure 4), wax was then added to complete both form and function (Figure 5 and Figure 6). This additive/reductive model operates as the essential blueprint for the provisional and, ultimately, for the definitive restorations (Figure 7).
Provisionalization
As the procedure was an additive restorative technique, little tooth structure was removed before introducing provisionals (Figure 8). Impressions were taken using impression trays (Directed Flow Impression Trays™, 3M ESPE) filled with a heavy-body impression material (Imprint™ 3). A bite jig was created from a rigid PVS bite registration material (MegaBite®, Discus Dental, www.discusdental.com) on the articulated wax-up of the molars and it was used to maintain the correct proposed vertical dimension throughout the procedure. Both the right and left bite registrations were used for bite verification and to maintain correct vertical dimension. The ceramist also used the bite jig to mount the upper and lower preparation models to the proper vertical dimension. Stump shades (Ivoclar Vivadent) and digital photographs were taken to provide the laboratory with case specifics (Figure 9).
Provisional restorations were created based on the additive/reductive model. Photographs were taken and models of the provisionals were created. Once the patient was satisfied with the results of the provisionals, all photographs and necessary diagnostic information were forwarded to the laboratory with a prescription for IPS e.max Press restorations (ie, cut-back and layered veneers) for the anteriors (Figure 10).
Laboratory Fabrication
To meet the requirements of the patient’s form and function, the laboratory technician must have all diagnostic tools necessary to complete the case. The foundation of any case should be world-class model work. This foundation is crucial to achieve results synonymous with this level of dentistry, especially full-mouth reconstructions. Other diagnostic tools required to reach this level include preoperative, postoperative, and provisional photographs; master impressions; provisional impressions; a CR bite registration; and a stick bite. It is of the utmost importance to have either an eyebrow-to-chin photograph of the patient—with the stick bite in place on the lower incisors to communicate the horizontal plane in relation to the patient’s face—or an eyebrow-to-chin photograph with a grid overlay.
After receiving the provisional records, impressions, and eyebrow-to-chin photographs of the patient smiling with his provisionals (fabricated in plastic), a Sil-Tech® matrix (Ivoclar Vivadent) was formed over the cast of the provisionals and placed in a pressure chamber. This matrix was then used as a mold to inject wax onto the treated and lubricated master dies (Figure 11). Through the lost-wax process, the final restorations were produced using lithium-disilicate glass-ceramic (IPS e.max Press) HT BL1 ingots pressed at a temperature of 917°C (Figure 12 and Figure 13).
After pressing, divesting, and fitting the IPS e.max restorations, the facial surfaces were cut back 0.5 mm incisally to 0.2 mm cervically. A guaranteed halo was embossed around the outer silhouette of the incisal half, and stains were added to mimic the high and low values of the patient’s natural internal tooth structure (Figure 14 and Figure 15). After the stains were fired, internal effect powders were added to emulate a natural tooth with the enamel removed, then fired. Next, the restorations were segmentally enameled and fired. Finally, the facial lobes and surface texture characteristics of a natural tooth’s surface were created. The restorations were then glazed, polished, and ready for delivery.
Final Seating
The provisionals were removed and the preparations were cleaned. The final restorations were tried in with a try-in cement gel (Variolink® Veneer, Ivoclar Vivadent) to verify fit, occlusal contacts, and patient satisfaction. The patient was pleased with the results, after which proper adhesive protocols were followed by permanent cementation of the restorations, using All Bond® 3 (BISCO, www.bisco.com) for adhering the restorations and Variolink Veneer cement for bonding teeth.
The molars remained out of occlusion at this point because they were planned for the final treatment stage. The remaining stages of the full-mouth reconstruction (ie, phase 2, teeth Nos. 20 through 29; and phase 3, the molars) were completed following the same procedure. At the conclusion of the case, the patient, dentist, and technician were pleased with the esthetic and functional treatment results (Figure 16).
When fabricating full-mouth restorations, the forces resulting in the wear, breakage, joint dysfunction, or malocclusion should be considered. The goal of occlusal dentistry is to balance the masticatory stresses to prevent uneven and excessive contacts from breaking down dentition.15 Several issues need to be assessed—and resolved if necessary—to restore a stable and balanced occlusion, including TMJ dysfunction, occlusal vertical dimension, anterior guidance, performance of the masticatory musculature, and condylar function. The type of wear can help determine the underlying causes and the appropriate treatment. Therefore, ceramists and dentists providing full-mouth rehabilitations should possess an in-depth knowledge of occlusal principles in order to provide predictable, reliable, and long-lasting restorations.
1. Bartlett DW. The role of erosion in tooth wear; aetiology, prevention and management. Int Dent J. 2005;55(4 Suppl 1):277-284.
2. Dawson P. Functional Occlusion From TMJ to Smile Design. Canada: Mosby, Inc.; 2007.
3. The Glossary of Prosthodontic Terms. J Prosthet Dent. 1999;81(8):39-110.
4. Sorensen JA, Cruz M, Mito WT, Raffeiner O, et al. A clinical investigation on three-unit fixed partial dentures fabricated with a dual-curing adhesive system and a self-curing resin cement. Pract Periodontics Aesthet Dent. 2006;8
6):427-431.
5. Höland W, Schweiger M, Frank M, Rheinberger V. A comparison of the microstructure and properties of the IPS Empress 2 and the IPS Empress glass-ceramics. J Biomed Mater Res. 2000;53(4):297-303.
6. Kheradmandan S, Koutayas SO, Bernhard M, Strub JR. Fracture strength of four different types of anterior 3-unit bridges after thermo-mechanical fatigue in the dual-axis chewing simulator. J Oral Rehabil. 2001;28(4):361-369.
7. Guess PC, Zavaneeli RA, Silvia NR, et al. Monolithic CAD/CAM lithium disilicate versus veneered Y-TZP crowns:comparison of failure modes and reliability after fatigue. Int J Prosthodont. 2010;23(5):434-442.
8. Hoofard, S, Wehrkamp S. Pressed esthetics: creating highly esthetic pressed veneers using Ivoclar Vivadent’s IPS e.max Press lithium disilicate. dlpmagazine.com. 2010;1-6.
9. Tysowsky GW. The science behind lithium disilicate: a metal-free alternative. Dent Today. 2009;28(3):112-113.
10. Reynolds JA, Roberts M. Lithium-disilicate pressed veneers for diastema closure. Inside Dentistry. 2010;6(5):46-52.
11. Helvey GA. Chairside C. Lithium-disilicate restoration for anterior teeth made simple. Inside Dentistry. 2009;5(10):58-66.
12. McLaren EA, Phong TC. Ceramics in dentistry: classes of materials. Inside Dentistry. 2009;5(9):94-103.
13. Ritter RG, Culp L. Ingot selection for aesthetic restorations using contemporary pressed ceramics. Pract Proced Aesthet Dent. 2002;14(6):472-478; quiz 470.
14. Spear FM. Approaches to vertical dimension. Inside Dentistry. 2007;3(7):34-44.
15. DiMatteo AM. Pounding on the occlusion pulpit. Inside Dentistry. 2008;4(3):102-110.
For product information on Laboratory Services, visit: dentalaegis.com/go/id423
To read another article about Laboratory Communication, visit: dentalaegis.com/go/id424
Brent Engelberg, DDS
Private Practice
Arlington Heights, Illinois
Brad Jones, FAACD
Owner
Smile, Inc.
Boise, Idaho