An efficient, cost-effective approach for long-term success
Samuel M. Strong, DDS
Implant overdentures can be retained either by attachments that snap onto or into a bar or by connecting directly to abutments threaded into the implants.1 Both modalities have advantages and disadvantages and, to some extent, the decision to choose between bar or attachment-only retention is made from a series of technical factors, including the number of implants placed, implant size and angulation, interarch space, bone density, and hygiene maintenance factors.2-9
Use of either implant retention form has been shown to provide higher levels of patient satisfaction compared with conventional full dentures.10-13
Incorporating CAD/CAM technology into the overdenture process allows the clinician and lab technician to design, view, and modify the proposed retention bar on the computer monitor without the more laborious process of bar wax-up and casting. The entire procedure from design to fabrication is accomplished faster and more cost effectively than previous laboratory techniques.
The patient was a 67-year-old woman who had been totally edentulous in both arches for more than 20 years. Her experience with conventional removable full dentures had been quite satisfactory during most of this time. However, severe alveolar atrophy eventually made her denture retention unsatisfactory with instability during function and speaking.
Fixed and removable implant options were presented to the patient. For financial reasons, she chose an option to have four implants placed in each arch for attachment-retained overdentures.
A maxillary transitional conventional removable denture was fabricated and placed at the time of sinus grafting due to the expected expansion of the maxilla.14 The surgical dentist advocated waiting 6 months after the maxillary sinus lift grafts before placing the maxillary implants. The mandibular implants were placed simultaneously at the time of the grafts. However, only three implants (NobelReplace®, Nobel Biocare, www.nobelbiocare.com) were placed due to mandibular atrophy of the residual alveolus. The implants were placed relatively parallel to each other, an important factor for increased longevity of the attachments used for a stand-alone attachment–retained overdenture.15
Master Implant Level Impression
Three months after the lower implants were placed, the mandibular implants were torque-tested to the recommended 35-Ncm force and found to be successfully integrated. The master implant level impression was made using a custom-molded Strong-Massad Denplant™ impression tray (Nobilium, www.cmpindustries.com) and Aquasil Ultra impression material (DENTSPLY Caulk, www.caulk.com).
Two of the three mandibular implants were NobelReplace 3.5-mm diameter implants (narrow platform). These implants were placed bilaterally in about the first bicuspid positions. The center implant placed was a 4.3-mm diameter NobelReplace (regular platform) (Figure 1). Because there were only three mandibular implants rather than the planned four, and because of the narrow diameter of two of them, the original treatment plan was altered. A bar-retained overdenture plan was substituted for the original attachment-only plan. The splinting action of the bar-retained overdenture was deemed a better structural support system for this case than the stand-alone, attachment-only format.16
The dental lab fabricated an acrylic verification jig (AVJ) on the mandibular master cast. The AVJ is an acrylic light-cured bar connected with metal abutments into the three implant analogs on the master cast. This was used at the second appointment to confirm the accuracy of the master cast.
AVJ Confirmation, Face-Bow Transfer, Jaw Relation Records
The AVJ was tried in using the Sheffield (one-screw) test. The AVJ was first fastened to only one of the two posterior implants. After pressing down along its length, no movement of the AVJ was noted, confirming that all three of the metal abutment portions fit completely on the three implants. The screw site was changed to the opposite end of the AVJ, and the test repeated, again with no movement of the AVJ noted upon finger pressure across the top of its surface. In addition, a radiograph of the AVJ confirmed complete seating of the metal abutments into the implants.
A face-bow transfer was used to mount the maxillary denture model to the upper member of the Denar® Mark 330 articulator (Whip Mix Corporation, www.whipmix.com).
Next, the Massad Jaw Relation Recorder (Nobilium) was used to record centric relation at the correct occlusal vertical dimension. The recorder consists of a separate upper striking plate, bonded to the palatal portion of the upper denture base, and a lower tracing pin and holder luted to a light-cured baseplate17 (Figure 2).
The process of recording centric relation included:
• finding physiologic rest position.
• finding occlusal vertical dimension.
• establishing centric relation tracing.
• connecting the upper and lower baseplates in centric relation at the correct vertical dimension.
Physiologic rest position was found by having the patient inhale and exhale deeply several times followed by allowing the jaws to come to rest with the lips slightly separated. A marking pen was used to place dots on the patient’s chin and nose. As the patient came to “rest” after each exhalation, the distance between the chin and nose dots was measured with a Boley gauge. This procedure was repeated until the distance measured dot-to-dot was exactly the same for at least five repetitions. This measurement represented the patient’s physiologic rest position.
The maxillary baseplate/striking plate and mandibular pin holder/pin assembly were next inserted intraorally. The patient closed together with the lower pin touching the maxillary striking plate. At this closure, the dot-to-dot distance between chin and nose was remeasured. The pin’s position in the ball-bearing nut can be lowered or raised by rotating the pin clockwise or counterclockwise. The patient’s closure of pin against striking plate was measured until the distance dot-to-dot was approximately 4 mm less than the measured physiologic rest position. This “closed” position represented the patient’s occlusal vertical dimension. Expressed alternatively, the patient closed through her proposed freeway space from physiologic rest position to OVD.
The upper striking plate surface was colored with a marking pen prior to intraoral insertion. With the patient closed to the desired OVD, she then rubbed the lower pin against the striking plate by moving her mandible forward and backward and side to side. These actions of mandibular movements scribed an arrow on the black colored striking plate. The tip of this arrow, or tracing, represented her centric relation position (Figure 3). A plastic pin receiver disc with a central hole was luted with sticky wax directly over the tip of the arrow. With the patient closed into the plastic disc hole over the arrow tip, the maxillary and mandibular baseplates were connected intraorally by injecting bite registration material between them and around the pin. Thus the patient’s centric relation position was captured at the correct OVD. Using the jaw relation recording, the lower master cast was mounted to the upper cast on the Denar Mark 330 articulator.
Mandibular Wax Try-in and CAD/CAM Fabrication
At the commercial dental lab (Green Dental Lab www.greendentallab.com), denture teeth were set in wax and returned to our office for an intraoral try-in. At this try-in appointment, the occlusal relationship between the mandibular setup and the existing maxillary denture was found to be excellent. Articulating paper confirmed the patient’s perception that both right and left sides contacted simultaneously. Cuspid disclusion was also noted when the patient moved the mandible into right and left excursive motions. Phonetics and esthetics of the setup were approved by both the author and the patient. The setup was then returned to the dental lab for bar fabrication.
A CAD/CAM format was chosen to splint the implants together due to the efficiency in bar design and accuracy afforded with this approach.19-22 Using CAD/CAM software and a digital scanner (NobelProcera™, Nobel Biocare), the proposed bar design was created on the computer. The approved mandibular denture setup was also scanned and superimposed over the bar on the computer (Figure 4 and Figure 5). The computer image allowed the dental team to design and visualize the bar with a minimum of 2-mm space from the bottom of the bar to the edentulous ridge for ease of cleaning by the patient.23
Previously, a laboratory-produced wax-up of the bar would be scanned to establish an electronic file for the bar. With the CAD/CAM technology used in this case, however, all of this work is done virtually with the computer software, reducing lab time and expense. The author and denture lab technician approved the computer-generated bar design that was then sent as an electronic file to the milling facility. The bar was fabricated by robotic milling of a solid titanium disc to the dimensional specifications of the electronic file. The bar was then polished and returned to the dental lab.
LOCATOR® abutment receptacles (Zest Anchors, www.zestanchors.com) were tapped and drilled at the lab. Locator abutments were threaded into these sites24,25 (Figure 6). A strengthening cast framework was made as a sleeve over the bar and inserted into the intaglia of the baseplate as well as Locator metal housings and attachments. The framework reduces the potential for denture base fracture as it ages and fatigues.26
Bar Try-In
The bar and mandibular denture setup were returned to our office for try-in (Figure 7). At the bar try-in appointment, the Sheffield test was used to confirm complete seating and also verified with a panoramic radiograph.
The denture setup with Locator attachments was seated onto the bar. Occlusion, esthetics, phonetics, and retention were evaluated and approved by the patient and the author.
Mandibular Overdenture Delivery
The case was processed and returned to our office for delivery (Figure 8). The four Locator metal housings and attachments were processed into the denture base by the dental lab (Figure 9).
Occlusion was checked and needed minimal adjustment to achieve simultaneous contact with the posterior teeth when the patient closed into centric relation. Cuspid disclusion was also observed with mandibular eccentric movements. Phonetics and esthetics were approved by the patient and the author prior to dismissal.
The patient was instructed on insertion and removal of the overdenture. Two blue (1-lb) anterior attachments and two black (processing) attachments were deemed adequate for initial stability and retention during the first few weeks of acclimation. One month after insertion, the two black posterior attachments were removed and two blue (1-lb) attachments were placed into the housings already cured into these posterior sites. The patient confirmed complete satisfaction with overdenture retention.
The use of a bar to splint the three implants together affords a structural support system conducive to long-term success with only three implants. It is possible that similar success could be achieved using a stand-alone attachment format. However, due to the small diameter size of two of the three implants, the advantages of splinting were considered to be of enough benefit to employ the bar.
Six months after the maxillary bone grafting procedure, four NobelActive (Nobel Biocare) implants (4.3 mm x 13 mm) were placed in the maxilla. The surgical dentist graded the bone density of the maxillary alveolus as D3, or soft bone, at the time of implant placement. Therefore, it was decided to construct the maxillary overdenture with bar-splinted implants in the same fashion as the mandibular overdenture. However, the maxillary case was designed with two separate bars splinting the right side implants (No. 3 and No. 6) and left side implants (No. 10 and No. 14) (Figure 10). This design allowed for Locator abutments to be placed in the middle and mesial aspects of each bar. In addition, the passivity of the two shorter bars was facilitated versus making one long-span bar fit passively.
The maxillary bar overdenture appointments were completed in the same sequence previously noted for construction of the mandibular overdenture. An AVJ was tested intraorally to confirm the accuracy of the master model and implant replicas positions using the Sheffield test. Centric relation records at the desired OVD were procured using the Massad Jaw Recorder to mount a model of the new mandibular overdenture to the maxillary master cast on the semi-adjustable articulator.
A maxillary overdenture setup was approved for phonetics, esthetics, and occlusal relationships followed by fabrication of the two CAD/CAM titanium bars. The Sheffield test confirmed passivity of fit of the bars intraorally and the maxillary overdenture was processed and delivered (Figure 11 through Figure 13).
At subsequent appointments, the patient has confirmed her complete satisfaction with the retention, function, and esthetics afforded her with the bar-retained overdentures.
The use of CAD/CAM virtual technology in cases including overdenture bars represents an exciting new approach to design and fabrication for both the clinician and lab technician. Inaccuracies encountered with traditional wax and cast alloy bars are avoided with the computer usage and robotic milling precision. The accuracy of the CAD/CAM bar format provides a precision, passive fit essential to the long-term success of the overdenture case.
The author is a stock shareholder of Global Dental Impression Trays, Inc. and a speaker for Nobel Biocare.
1. Strong SM. Removable implant-retained overdentures: a case report. Dent Today. 2009;28(5):74-79.
2. Batenburg RH, Meijer HJ, Raghoebar GM, Vissink A. Treatment concept for mandibular overdentures supported by endosseous implants: a literature review. Int J Oral Maxillofac Implants. 1998;13(4):539-545.
3. Trakas T, Michalakis K, Kang K, Hirayama H. Attachment system for implant retained overdentures: a literature review. Implant Dent. 2006;15(1):24-34.
4. Fueki K, Kimoto K, Ogawa T, Garrett NR. Effect of implant-supported or retained dentures on masticatory performance: a systemic review. J Prosthet Dent. 2007;98(6):470-477.
5. Narhi TO, Hevinga M, Voorsmit RA, Kalk W. Maxillary overdentures retained by splinted and unsplinted implants: a retrospective study. Int J Oral Maxillofac Implants. 2001;16(2):259-266.
6. Mericske-Stern RD, Zarb GA. Clinical protocol for treatment with implant-supported overdentures. In: Bolender CE, Zarb Ga, Carlsson GE, eds. Boucher’s Prosthodontic Treatment for Edentulous Patients. 12th ed. St. Louis, MO: Mosby;1997:527.
7. Naert I, Quirynen M, Hooghe M, van Steenberghe D. A comparative prospective study of splinted and unsplinted Branemark implants in mandibular overdenture therapy: a preliminary report. J Prosthet Dent. 1994;
71(5):486-492.
8. Pasciuta M, Grossmann Y, Finger IM. A prosthetic solution to restoring the edentulous mandible with limited interarch space using an implant-tissue-supported overdenture: a clinical report. J Prosthet Dent. 2005;93(2):116-120.
9. Assad AS, Abd El-Dayem MA, Madawy MM. Comparison between mainly mucosa-supported and combined mucosa-implant-supported mandibular overdentures. Implant Dent. 2004;13(4):386-392.
10. Karabuda C, Yaltirik M, Bayraktar M. A clinical comparison of prosthetic complications of implant-supported overdentures with different attachment systems. Implant Dent. 2008;17(1):74-81.
11. Awad MA, Lund JP, Dufresne E, Feine JS. Comparing the efficacy of mandibular implant-retained overdentures and conventional dentures in middle aged edentulous patients: satisfaction and functional assessment. Int J Prosthodont. 2003;16(2):117-122.
12. Burns DR, Unger JW, Elswick RK Jr, Giglio JA. Prospective clinical evaluation of mandibular overdentures: Part II—patient satisfaction and preferences. J Prosthet Dent. 1995;73(4):319-325.
13. Boerrigter EM, Geertman ME, Van Oort RP, et al. Patient satisfaction with implant-retained mandibular overdentures. A comparison with new complete dentures not retained by implants--a multicentre randomized clinical trial. Br J Oral Maxillofac Surg. 1995;33(5):282-288.
14. Strong S. Transitional removable dentures. Gen Dent. 2010;58(3):171-174.
15. Al-Ghafli S, Michalakis KX, Hirayama H, Kang K. The in vitro effect of different implant angulations and cyclic dislodgement on the retentive properties of an overdenture attachment system. J Prosthet Dent. 2009;102(3):140-147.
16. Slot W, Raghoebar GM, Vissink A, et al. A systematic review of implant-supported maxillary overdentures after a mean observation period of at least 1 year. J Clin Periodontal. 2010;37(1):98-110.
17. Strong SM. Attachment-retained overdentures: the most cost-effective implant solution for the edentulous arch. Gen Dent. 2009;57(2):112-117.
18. Massad JJ, Cagna D, Lobel W, Thornton J. Complete denture prosthodontics: modern approaches to old concerns. Inside Dentistry. 2008;4(8):84-93.
19. Bueno-Samper A, Hernandez-Aliaga M, Calvo-Guirado JL. The implant-supported milled bar overdenture: a literature review. Med Oral Patol Oral Cir Bucal. 2010;15(2):375-378.
20. Karimi-Boushehri F, Cable C. Advanced implant overdenture superstructure treatment planning with computer-assisted design systems. Int J Comput Dent. 2010;13(1):57-65.
21. Reshad M, Cascione D, Aalam AA. Fabrication of the mandibular implant-supported fixed restoration using CAD/CAM technology: a clinical report. J Prosthet Dent. 2009;102(5):271-278.
22. Landa LS, Cho SC, Froum SJ, et al. A prospective 2-year clinical evaluation of overdentures attached to nonsplinted implants utilizing ERA attachments. Pract Proced Aesthet Dent. 2001;13(2):151-156.
23. Misch CE. Contemporary Implant Dentistry. 2nd ed. St. Louis, MO: Mosby; 1998:175-192.
24. Buttel AE, Buhler NM, Marinello CP. Locator or ball attachment: a guide for clinical decision making. Schweiz Monatsschr Zahnmed. 2009:119(9):901-918.
25. Strong SM. Conversion from bar-retained to attachment-retained implant overdenture. Dent Today. 2006;25(1):66-70.
26. Piermatti J, Winkler S. Metal bases for implant overdentures. Gen Dent. 2010;58(5):400-403.
Samuel M. Strong, DDS
Private Practice
Little Rock, Arkansas
Adjunct Professor
General Practice Residency
University of Arkansas for Medical Sciences
Little Rock, Arkansas
Diplomate
International Congress of Oral Implantologists


Figure 1 Figure 2 Figure 3
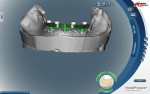

Figure 4 Figure 5 Figure 6


Figure 7 Figure 8 Figure 9


Figure 10 Figure 11 Figure 12
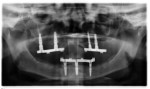
Figure 13