Using a digital workflow to increase efficiency and produce superior results
By Grady Crosslin, CDT
Today, digital workflows have allowed dental laboratory technicians to maximize the efficiency of their teams while simultaneously providing clinicians and patients with products superior to those produced using analog methods. The increasing popularity of digital technologies has changed the type of restorations available, as well as the method used by the dental laboratory to create and deliver them. By incorporating a digital system that delivers an efficient workflow, technicians can create high-quality tooth-borne restorations and implant-borne customized abutments that can, in turn, reduce complications and enhance the communication within the interdisciplinary team.
In this particular case, the patient presented with failing dentition on teeth Nos. 7 through 10 (Figure 1). The entire treatment team used digital technology to create a thorough case plan; this included immediate customized temporary abutments and a framework to be delivered at the time of implant surgery for sites 7 and 10, as well as a final 4-unit, porcelain-fused-to-zirconia bridge for delivery upon completion of osseointegration and healing.
An integrated digital workflow platform consisting of guided surgery software, intraoral scanning, and CAD/CAM technology facilitated proper treatment planning for the entire team. Overlaying guided surgery treatment plans with intraoral scan files into a CAD/CAM system provided the dental team with an ideal opportunity to review planned implant placement and its impact on the design and delivery of the temporary and final restorations. Adjustments, if any, could be made as a team prior to the implant surgery and the “top-down” treatment approach was executed with the patient’s final smile in mind.
The process began by taking an intraoral scan. Then, coDiagnostiX™ guided surgery software by Dental Wings (www.dental-wings.com) was used to get an accurate picture of available bone and neighboring dentition. The surgeon then decided to proceed with the tooth extraction followed by immediate placement of 3.3 x 14 Straumann® Roxolid® Implants in sites 7 and 10 with a non-invasive flapless procedure. The light blue line represents the scan of the wax-up and proposed prosthetic solution (Figure 2).
A diagnostic (light blue image) wax-up, which was scanned by the Straumann CS2 in-lab scanner (www.straumann.us), was used to generate a .stl file that was overlaid with the coDiagnostiX scan (dark blue image) and an Align Technology iTero® (www.aligntech.com) digital impression file to visualize the current dentition and facilitate planning for the ideal restorative outcome (Figure 3).
With the aid of this technology, the laboratory technicians were able to fabricate a surgical guide and design customized temporary abutments and the provisional framework prior to the time of surgery. Due to the position of the implant, they fabricated a screw-cemented temporary, which allowed them to cement the bridge over the customized temporary abutments intraorally, but left the screw access holes open for ease of cleaning and later removal for the final restoration (Figure 4).
At the time of surgery, implant placement in sites 7 and 10 proceeded as planned. Following the pre-surgical plan developed by the treatment team, customized temporary abutments were seated and a 4-unit temporary bridge was cemented in place (Figure 5 through Figure 7).
Four months later, following implant osseointegration and healing, a closed-tray impression was taken and models were prepared. The models were scanned in the Straumann CS2 in-lab scanner to facilitate the design of the final prosthesis (Figure 8). Straumann CARES® Titanium Abutments were designed in the CARES® Visual 8.0 Software for Nos. 7 and 10 (Figure 9).
Shortly thereafter, CARES Titanium Abutments were received at the laboratory from the Straumann Centralized Milling Facility in Arlington, Texas. The technician rescanned the model and final abutments to design the zerion® LT framework (Straumann) (Figure 10 through Figure 12).
Once the zerion LT framework was received at the laboratory from the Straumann Centralized Milling Facility in Arlington, Texas, its fit was verified on a model. Porcelain was applied with the appropriate shade and contour, and seating jigs were made for proper intraoral abutment placement. Following these steps, all of the prosthetics were delivered to the restorative dentist for try-in and final cementation (Figure 13).
The successful integration of three technologies—guided surgery software, intraoral scanners, and CAD/CAM software—allowed the dental team to deliver an ideal functional and esthetic temporary prosthetic solution to the patients at the time of surgery. Successful pre-planning through technology and teamwork is imperative to achieve the desired end result. Laboratory technicians who can use technology to deliver a temporary prosthesis at the time of surgery deliver immense value to the entire dental team and make it more likely that the patient will leave implant placement surgery with a smile. Incorporating immediate temporary prostheses facilitates tissue sculpting and the shaping of the smile line during the transition to the final prosthetic device. Their importance to a successful treatment plan should not be overlooked.
Surgery performed by Dr. David Feinerman. Dentistry by Dr. Janice Luke. Planning, design, and fabrication of all prosthetics by Crosslin’s Creative Ceramics.
Grady Crosslin, CDT is the founder of Crosslin Creative Ceramics in Weatherford, TX and West Palm Beach, FL.
For more information, contact:
Straumann
P 800-448-8168
W www.strauman.us
E [email protected]
The preceding material was provided by the manufacturer. The statements and opinions contained therein are solely those of the manufacturer and not of the editors, publisher, or the Editorial Board of Inside Dental Technology.

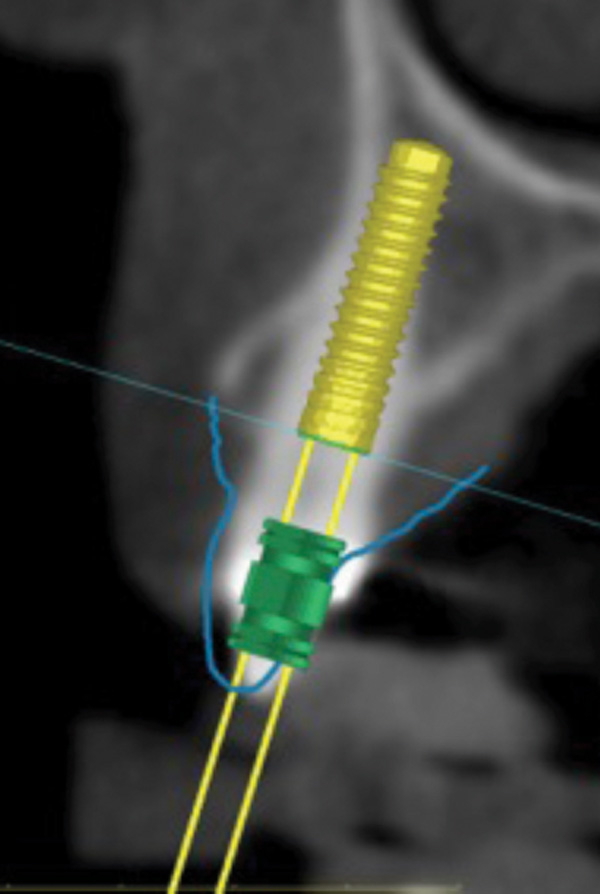
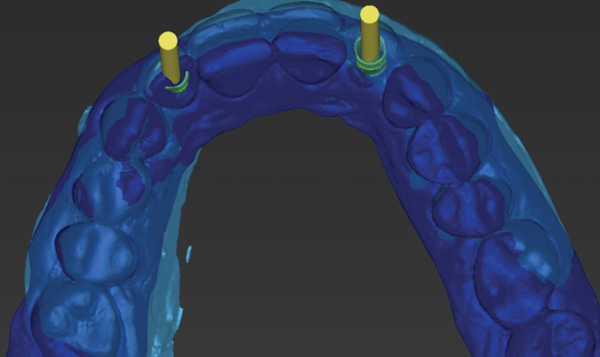
 Image 4 of 13Figure 4 Screw access holes were left open to facilitate both the cleaning and later removal of the temporary prosthesis.
Image 4 of 13Figure 4 Screw access holes were left open to facilitate both the cleaning and later removal of the temporary prosthesis.


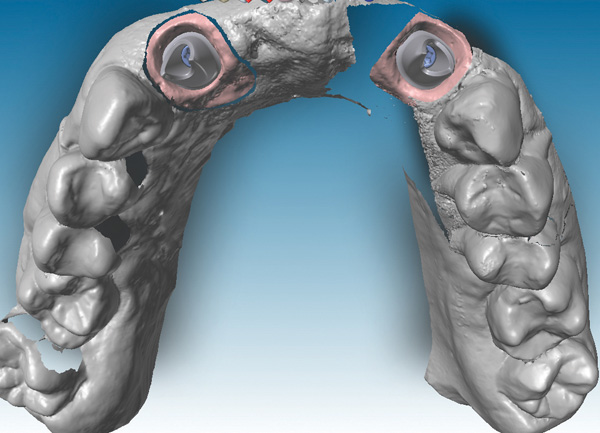
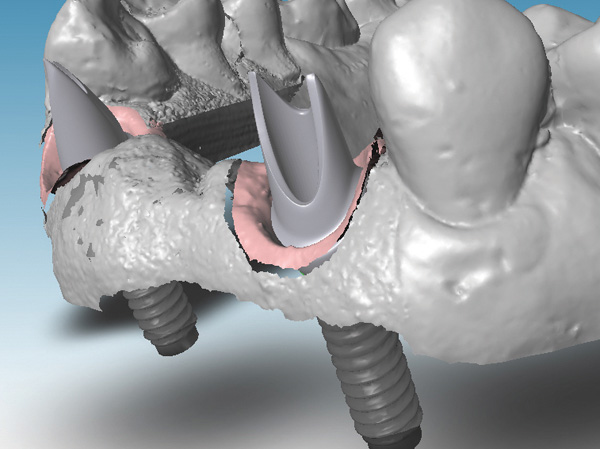
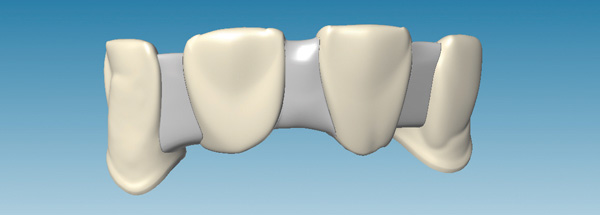
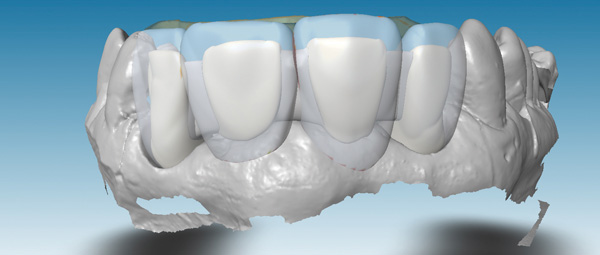

 Image 13 of 13Figure 13 The final zirconia framework cemented in the mouth.
Image 13 of 13Figure 13 The final zirconia framework cemented in the mouth.