What these applications have meant for implant dentistry.
By Scott D. Ganz, DMD
Implant dentistry has been evolving rapidly over the past 20 years, in many instances becoming the first treatment alternative for missing teeth over a conventional fixed or removable prosthesis. It is widely recognized that patients do not come to dentists for implants, they want and need teeth to masticate food properly, and to restore deficient smiles. Why should a clinician offer a patient an implant alternative? Simply because it is still the only treatment alternative that replaces the root of the tooth—the new “root” that will support the new clinical “crown.” Often it is more than just the tooth that is missing. The surrounding soft tissue and supporting bone can be deficient as well, and adjunct procedures are recommended in addition to the placement of a dental implant to replace what is missing. In the past 25 years, the dental implant industry has been greatly amplified through ancillary procedures that enhance both surgical and prosthetic results. In the past 10 years, it is technology that has proven to be the most important catalyst to improving the level of accuracy, consistency, and overall care to our patients. Three major technologies that have had the most impact are cone-beam computed tomography (CBCT) imaging, guided-surgery applications, and CAD/CAM fabrication of restorative components.
The advent of medical CT imaging modalities for dentistry in the late 1980s allowed clinicians, for the first time, to visualize patient anatomy in three dimensions. In 1993, interactive treatment-planning software was introduced as an aid to assessing dental implant receptor sites.1 However, most clinicians and dental implant manufacturers did not jump into the “3D” pool. It was not until the development of lower-dose CBCT that the industry started to acknowledge the start of the digital age for dental implant diagnosis, treatment planning, and guided-surgery applications. For the first time, clinicians could image patients in their own office, and instantly assess the patient’s individual 3D anatomy. The key words here are “individual anatomy,” or the “reality of anatomy” that is specific and different for every patient. Besides the initial impact on private practice, today most dental schools have moved into the world of 3D imaging by acquiring CBCT machines. This is a major step forward in the evolution of the educational process for teaching maxillofacial anatomy, assessing pathology, impacted teeth, endodontics, orthognathic surgical applications, and dental implant reconstruction.
A conventional periapical radiograph provides only two-dimensional information to assess a given intraoral region.2-4 Therefore, the thickness of the buccal cortical plate, or the density of the bone, cannot be accurately determined. The path of the inferior alveolar nerve, the precise location of the mental foramen, the floor of the nose, and the dimensions of the maxillary sinus cannot be visualized with a high degree of accuracy with 2D imaging modalities when compared with 3D imaging afforded by CBCT.2,3 While digital radiographs allow for certain amount of enhancement through various software applications, the ability to manage 3D images of the maxillofacial region is unsurpassed.5
CBCT machines come with native software to acquire and process the vast amount of data required, and are aided by the increased computer power of today’s CPUs, on-board RAM memory, and fast graphic accelerator cards. This native software provides the clinician with the first glimpse into the patient’s 3D anatomy. For further refinement, third-party interactive treatment-planning software applications import the native Digital Imaging and Communication in Medicine (DICOM) data, and provide clinicians with a broad range of tools to plan a wider variety of procedures. The software empowers clinicians with an unprecedented ability to delve into a patient’s individual anatomy with a series of views built upon the CBCT data. An example of how the maxillary arch can appear in the axial, sagittal, coronal, and volumetric reconstructed views can be seen in Figure 1. Perhaps the most impressive view is the 3D reconstructed model of the arch, which can be rotated in any direction (Figure 2). Each of these views can be magnified and selectively navigated to assess the bone quality, clinical crown and root morphology, bone volume, adjacent vital structures, pathology, and other areas of interest. The ability to interactively assimilate all of these images in order to render an accurate diagnosis and treatment plan while reducing potential surgical and restorative complications is essential to achieving the maximum benefit of the technology.4-6
Many applications now contain a library of implants and restorative components supplied by dozens of manufacturers worldwide. An example of a 3D reconstruction of the maxilla can be seen in Figure 3. The bone has been made semi-transparent, revealing the adjacent tooth roots. The ability to assess root morphology and root trajectory can be an invaluable aid in the evaluation of an implant receptor site, as illustrated in the simulated placement of a realistic dental implant seen with navigational tools. While these exceptional images are highly useful, diagnosis and planning should include an understanding of all images provided by 3D patient data, such as the cross-sectional, panoramic, and axial slices. The cross-sectional image provides information related to the thickness of the buccal-lingual cortical plates, and vital structures in the area. The density of the bone can also be assessed by visualizing the grayscale levels, which provides important preoperative information. Realistic implants can be simulated within the available bone volume and manipulated within the potential receptor site as seen in Figure 4. The facial plate of bone is outlined in blue, and the thickness of the cortical bone can be visualized, and the distance from the outer aspect of the implant can be measured without distortion. Certain software also allows for the tooth to be simulated, so that the abutment projection (in yellow) can be visualized within the envelope of the “virtual” tooth.
The ability to separate individual anatomical structures or other entities based on varying the level of opacity has been labeled by the author as “selective transparency,” and provides invaluable information for planning dental implants.4 With today’s advanced software, a manufacturer-specific implant and abutment can be simulated within a “virtual occlusion” in order to achieve true restoratively driven treatment planning (Figure 5).6 Once the implant site has been selected, and the implant is properly positioned with the available bone, the clinician can choose to place the implant freehand according to landmark measurements, or by using a surgical template fabricated for a guided surgical approach. Many templates are fabricated though a process known as “stereolithography” or rapid prototyping, taking the simulated plan and converting the dataset into a laser-cured resin pattern. Templates can be tooth-borne, mucosal-borne, or bone-born, providing a full range of surgical options for any level of intervention.7-12 A recent publication indicated that there were no differences in the accuracy of implant placement with mucosal-supported guides fabricated from CT as compared with lower-radiation CBCT.8 However, it should be noted that the template will only be as good as the plan, emphasizing the importance of the diagnosis and treatment-planning phase. Other applications that can be enhanced through 3D simulation include sinus augmentation procedures, block bone grafts, third-molar and impacted tooth extractions, ridge splitting, and orthognathic surgery.13
To illustrate the versatility of digital imaging, another novel concept is to appreciate a mandibular arch with a high and thin alveolus where the anterior segment requires reduction for denture fabrication or implants (Figure 6). Software simulation can help plan exactly how much bone needs to be removed to widen the alveolus for later implant placement (Figure 7). To treatment plan the bone removal, the 3D reconstruction can be “sectioned” virtually (Figure 8). To facilitate the surgery, an intraoperative “bone reduction” template can be fabricated to provide accurate sectioning at the time of surgery (Figure 9).6 The alveolus can, therefore, be widened adequately for the placement of implants in strategic positions within the most volume of bone in the anterior symphysis.
Simultaneous with the development of CT imaging modalities, the application of CAD/CAM technology also has been evolving to enhance the accuracy and consistency of conventional restorative dentistry. Advances in software, hardware, and materials have changed both the chairside and laboratory side of the dental restorative workflow. In the author’s opinion, the conventional “lost-wax” casting method may become totally obsolete in the very near future forcing dental laboratory technicians to move from the Bunsen burner to the new virtual tools on the computer. Additionally, the advent of extraoral and intraoral optical scanning technology has penetrated the marketplace with a series of solutions by major dental manufacturers to capture tooth preparations digitally instead of using the old analog method. The restorative process of dental implants has been greatly enhanced by significant innovation in the area of custom CAD/CAM abutments, milled bars, and milled superstructures.14,15
To achieve the desired emergence profile once an implant has been placed, conventional technology called for the use of a custom-cast post, creating with a waxing sleeve and a machined base to interface with the implant. Evolving technology first provided a solution where a solid piece of titanium was milled to the proper contours and emergence profile while accurately fitting to the implant through a CAD/CAM process.15-17 Once custom titanium abutments were proven to be consistently accurate and cost-effective, the next choice was to create a more esthetic result. Using state-of-the-art software, custom zirconia abutments are now designed on the computer and milled to the individual specifications of the receptor site (Figure 10). The margin interface, scalloped interproximal design, and emergence profile can be controlled to the highest tolerances (Figure 11).15-17 To complement the esthetic result, a CAD/CAM zirconia crown could be fabricated.
Technology has affected all aspects of how dental care is delivered, and perhaps no area has been impacted more than dental implants. From the initial radiographic image acquisition to interactive treatment planning software, guided surgery, and the ability to deliver customized abutments through improved CAD/CAM technology is changing the way that implants are placed and restored today (Figure 12). Further applications of intraoral optical scanning, digital impressions, combined with CBCT data collection will provide the foundation for future innovation.19-20
1. Rothman SLG. Interactive Implant Surgical Planning with SIM/Plant. In: Rothman SLG, ed. Dental Applications of Computerized Tomography. Chicago, IL: Quintessence, 1998:139-152.
2. Sonick M, Abrahms J, Faiella R. A comparison of the accuracy of periapical, panoramic, and computerized tomographic radiographs in locating mandibular canal . Int J Oral Maxillofac Implants. 1994;9:455-460.
3. Lam EW, Ruprecht A, Yang J. Comparison of two-dimensional orthoradially reformatted computed tomography and panoramic radiography for dental implant treatment planning . J Prosth Dent. 1995;74:42-46.
4. Ganz SD. Cone beam computed tomography—assisted treatment planning concepts . Dent Clin N Am. 2011;55(3):515-536.
5. Ganz SD. Implant complications associated with two- and three-dimensional diagnostic imaging technologies. In: Dental Implant Complications—Etiology, Prevention, and Treatment. Froum SJ, ed. Wiley-Blackwell. UK, West Sussex; 2010:71-99.
6. Ganz SD. Techniques for the use of CT imaging for the fabrication of surgical guides . Atlas Oral Maxillofac Surg Clin North Am. 2006;14:75-97.
7. Tardieu PB. Scanning appliances and virtual teeth. In: The Art of Computer Guided Implantology. Tardieu PB and Rosenfeld AL, eds. Quintessence, Hanover Park, IL: 2009:47-59.
8. Arisan V, Karabuda ZC, Piskin B, Ozdemir T. Conventional multi-slice computed tomography (CT) and cone-beam CT (CBCT) for computer-aided implant placement. Part II: reliability of mucosa-supported stereolithographic guides . Clin Implant Dent Relat Res. 2012;DOI10.1111/j.1708-8208.2011.00435.x. [Epub ahead of print].
9. Arisan V, Karabuda CZ, Ozdemir T. Implant surgery using bone- and mucosa-supported stereolithographic guides in totally edentulous jaws: surgical and post-operative outcomes of computer-aided vs. standard techniques . Clin Oral Implants Res. 2010;21(9):980-988.
10. Cassetta M, Giansanti M, DiMambro A, et al. Accuracy of two stereolithographic surgical templates: a retrospective study . Clin Implant Dent Relat Res. 2011;Jul11.DOI:10.1111/j.1708-8208.2011.00369.x. [Epub ahead of print].
11. Widmann G, Bale RJ. Accuracy in computer-aided implant surgery—a review . Int J Oral Maxillofac Implants. 2006;21(2):305-313.
12. DiGiacomo GA, Cury PR, de Araujo NS, et al. Clinical application of stereolithographic surgical guides for implant placement: preliminary results . J Periodontol. 2005;76(4):503-507.
13. Orentlicher G, Abboud M. The use of 3-dimensional imaging in dentoalveolar surgery . Compend Contin Educ Dent. 2011;32(5):78-86.
14. Kapos T, Ashy LM, Gallucci GO, et al. Computer-aided design and computer-assisted manufacturing in prosthetic implant dentistry . Int J Oral Maxillofac Implants. 2009;24(Suppl):110-117.
15. Kerstein RB, Castellucci F, Osorio J. Ideal gingival form with computer-generated permanent healing abutments . Compend Contin Educ Dent. 2000;21(10):793-802.
16. Kerstein RB, Radke J. A comparison of fabrication precision and mechanical reliability of 2 zirconia implant abutments . Int J Oral Maxillofac Implants. 2008;23(6):1029-1036.
17. Ganz SD. Computer-milled patient-specific abutments: Incredible quality with unprecedented simplicity . Pract Proced Aesthet Dent. 2003;15(8 Suppl):37-44.
18. Patel N. Integrating three-dimensional digital technologies for comprehensive implant dentistry . J Am Dent Assoc. 2010;141(Suppl 2):20S-24S.
For additional content on the Digital Imaging, visit:dentalaegis.com/go/id108
For information on Digital Imaging products, visit: dentalaegis.com/go/id109
Scott D. Ganz, DMD
Private Practice in Prosthodontics, Maxillofacial Prosthetics, and Implant Dentistry
Fort Lee, New Jersey


Figure 1 Figure 2 Figure 3

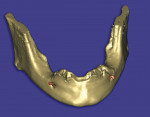
Figure 4 Figure 5 Figure 6
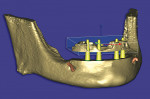
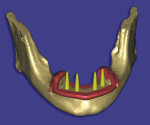
Figure 7 Figure 8 Figure 9
Figure 10